For many cancer survivors the treatments impact the lymphatic system, part of the circulatory system that is vital for immune function. Lymphedema is caused by a blockage of lymphatic system, and it is a long-term condition where excess fluid collects in tissues causing swelling (edema).
Lymphedema commonly affects one of the arms or legs. In some cases, both arms or both legs may be affected. Some patients might experience swelling in the head, genitals, or chest.
Exercise is an important tool in managing and preventing lymphedema, and we will cover top exercises that can help.
Lymphedema is one of the most overlooked topics amongst cancer patients.
Lymphedema is swelling produced by an accumulation of lymph fluid in the tissue. For breast cancer clients, the swelling occurs in the arm of the affected side due to damage to the lymph vessels in the armpit area caused by the removal of the axillary lymph nodes or from radiation to that area. for those of you who have had lymph nodes removed or irradiated elsewhere in your body, you will be at risk in that area as well as surrounding tissue.

Who is a candidate for lymphedema?
Anyone who has had radiation to or removal of the lymph nodes anywhere in their body is at risk for lymphedema
Other factors that increase your risk include:
* Being overweight
* Elderly
* In poor health
* Poor nutrition
* Infection
What are the stages of lymphedema?
STAGE 0 LYMPHEDEMA – Stage O lymphedema, which is also known as the latent or preclinical stage, is the newly added classification. At this stage the patient is at risk of developing lymphedema; however no swelling or other visible evidence of impaired lymph transport is present. Stage 0 can be present for months, or years, before any more serious signs appear.Studies have indicated that through the use of bioimpedance it is possible to identify changes in the at risk limb before they become visible. When changes develop, if specialized treatment is started immediately, it may be possible to prevent the development of further stages of lymphedema. (Bioimpedance is a non-invasive method of determining the composition of body tissues to evaluate the presence of body fluids such as lymphedema. Such measurements have been studies to establish a baseline at the time of breast cancer treatment.)
STAGE I LYMPHEDEMA – Stage I lymphedema is an early accumulation of fluid that is relatively high in protein content.
* There is visible swelling with this protein-rich lymph.
* This swelling can be temporarily reduced by elevation of the limb; however, the swelling soon returns when the limb is returned to a normal position.
* The swollen tissues are soft and pitting edema is present.
Lymphedema treatment should be begun as soon as signs are early detected. Waiting for the swelling to increase, or for an infection to develop, only makes the condition more difficult to treat. Prompt treatment of this stage can often control the condition and may prevent it from becoming more severe.
STAGE II LYMPHEDEMA – Stage II lymphedema is an increase in the swelling and a change in the tissues.
* Elevation of the limb will not reduce the swelling.
* The tissues become increasing firm due to fibrosis. Fibrosis is the formation of fine scar-like structures within the tissues that cause them to harden.
* Pressure against the limb produces only a slight indentation or in indentation at all.
* The tissue changes at this stage increase the risks of even greater swelling, fibrosis, infections, and skin problems.
* Stage II lymphedema can usually be improved with intense treatment.
STAGE III LYMPHEDEMA – Stage III lymphedema is also known as lymphostatic elephantiasis. It is a condition in which the tissue becomes extremely swollen and thickened due to a blockage in the flow of lymph and a buildup of fluid in tissues.
* The tissues become increasingly fibrotic (hardened). Pressure does not produce any pitting.
* Normal elasticity is lost and the skin hangs in folds.
* The skin may change color.
* Papillomas are small solid benign tumors that project above the surrounding tissue, may develop.
* Hyperkeratosis is an increase in the thickness of the outer layer of the skin, can develop.
* These changes in the texture of the skin are disfiguring and can limit mobility.
* Infections become more common because of increased risks of breaks in the skin. These infections include fungal infections and open wounds that form within the folds of skin.
With intense therapy, Stage III lymphedema can be improved and potentially be prevented from becoming worse; however, it is rarely reversed to an earlier stage.
One treatment to reduce the size of the limb is surgical debulking. Healing from this surgery can be difficult and, because the skin is still hardened, it still hangs in folds and deep creases are still present. These areas remain at risk for infections and open wounds
How can I minimize my risk for lymphedema?
* Avoid insect bites, burns, skin irritants, hangnails, and torn cuticles.
* Wear loose fitting clothing on affected area. Avoid tight fitting jewelry on the affected arm or hand Don’t overheat – avoid saunas, whirlpools, steam rooms, hot baths, and sun bathing.
* Don’t receive shots, have blood drawn, or have blood pressure taken on affected arm.
* If you are overweight and have experienced swelling, losing weight can help reduce it by reducing the amount of fatty tissue which retains fluid and blocks lymphatic pathways.
* Remember that tennis, racquetball, golf, and bowling are all considered risky sports for upper extremity lymphedema and that soccer, running, skating etc…. are risky sports for lower extremity lymphedema.
* Keep the at-risk area(s) spotlessly clean and use lotion after bathing.
* Avoid repetitive movements with the affected area.
* Avoid heavy lifting with the affected or at-risk arm. Never carry heavy handbags or bags with over-the-shoulder straps on the affected arm.
* When traveling by air, wear compression sleeves or stockings.
Lymph Drainage Exercises for Upper Extremity Lymphedema Prevention and Management
Prior to beginning these exercises, clients should start with a five-minute aerobic warm-up. As they begin each of the following exercises make sure to take several deep abdominal breaths (as were described earlier).
- Pelvic tilt – have your client/patient lie on their back with their knees bent and feet flat on the floor. Have them tilt their hips so that they are able to press the small of their back against the floor. Have them pause for several seconds then release the contraction. Repeat 5-10 times.
- Modified sit–up – have your client/patient lie on their back with their knees bent and feet flat on the floor. Instruct them to maintain a neutral pelvis. Have them keep their neck in neutral and their chin pointing to the ceiling. As they exhale, have them lift up their chest and shoulders, pausing when they feel their abdominal muscles tighten up. Have them slowly lower themselves back to starting position (trying not to rest between repetitions). Repeat as many times as they can comfortably
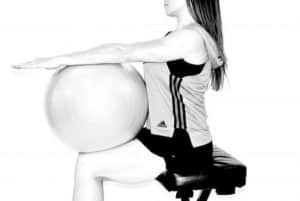
- **If your client/patient has a bad neck they can place a 55cm exercise ball on their stomach and against their bent legs. Keeping their arms straight and reaching toward ceiling, and their head relaxed on the floor, they should engage their abdominal muscles and press their arms against the ball. They can repeat this as many times as they can comfortably. This can also be done sitting upright in a chair (only the ball will be on their lap and their arms will be parallel to the floor) for someone who is unable to get to the ground.
- Neck stretches – refer to the neck stretches in the stretching section. These stretches can be done by the client/patient, or with assistance from the CES.
- Shoulder shrugs – have your client/patient shrug both shoulders, lifting them towards their ears as they inhale. Have them exhale, and depress their shoulders as low as they can (attempting to reach the floor with their fingertips) then return to a relaxed position. Repeat 5-10 times.
- Shoulder rolls – have your client/patient lift their shoulders up to the ears then rotate the shoulders back and down, making a smooth, continuous motion. Repeat 5-10 in each direction.
- Isometric shoulder blade squeeze – have your client/patient bend their elbows at 45-90 degrees out at their sides (parallel to the floor). Have them exhale and pull them towards the center of your back, squeezing the shoulder blades together. Pause. Have them inhale and return to starting position. Repeat 5-10 times.
- Isometric chest-press – have your client/patient place the palms of their hands together, with their elbows bent and arms at or below shoulder level. Have them exhale and push their hands firmly together. Pause. Have them inhale and relax. Repeat 5-10 times.
- Shoulder circles – have your client/patient hold their arms at or below shoulder height with their palms facing down. Have them make small circles with their arms (keeping arms elevated). Repeat 5-10 times in each direction.
- Wrist circles – have your client/patient hold their arms overhead and rotate their fist in small circles, isolating the movement to the wrist only. Rotate 5-10 times in each direction.
- Wrist flexion and extension – have your client/patient hold their arms overhead and flex and extend their wrists, isolating the movement to the wrist only. Repeat 5-10 times.
- Fist clench – have your client/patient hold their arms overhead and open their hands and stretch their fingers, spreading them apart. Then have them slowly clench each hand to make a fist. Pause. Repeat 5-10 times.
Lymph Drainage Exercises for Lower Extremity Lymphedema Prevention and Management
Prior to beginning these exercises, clients should start with a five-minute aerobic warm-up. As they begin each of the following exercises make sure to take several deep abdominal breaths (as were described earlier).
- Pelvic tilt – have your client/patient lie on their back with their knees bent and feet flat on the floor. Have them tilt their hips so that they are able to press the small of their back against the floor. Have them pause for several seconds then release the contraction. Repeat 5-10 times.
- Modified sit-up – have your client/patient lie on their back with their knees bent and feet flat on the floor. Instruct them to maintain a neutral pelvis. Have them keep their neck in neutral and their chin pointing to the ceiling. As they exhale, have them lift up their chest and shoulders, pausing when they feel their abdominal muscles tighten up. Have them slowly lower themselves back to starting position (trying not to rest between repetitions). Repeat as many times as they can comfortably.
**If your client/patient has a bad neck they can place a 55cm exercise ball on their stomach and against their bent legs. Keeping their arms straight and reaching toward ceiling, and their head relaxed on the floor, they should engage their abdominal muscles and press their arms against the ball. They can repeat this as many times as they can comfortably. This can also be done sitting upright in a chair (only the ball will be on their lap and their arms will be parallel to the floor) for someone who is unable to get to the ground.
- Bicycles – have your client/patient lie on their back with their knees bent at ninety degrees (shins are parallel to the floor). Instruct them to maintain a neutral pelvis and keep their upper body relaxed on the floor. They should raise their legs towards the ceiling, keeping the legs bent at about 45 degrees. Have them circle their legs like a bicycle 5-10 in each direction.
- Leg circles – have your client/patient lie on their back with left knee bent and foot on floor and right leg extended up toward the ceiling. Have them engage their abdominal muscles and “anchor” their hips to the floor as they perform clockwise and counter-clockwise hip circumduction, using very small and controlled movements, 5-10 times in each direction. Have them repeat the entire process on the other leg.
- Knee flexion/extension – have your client/patient lie on their back with both legs extended up toward the ceiling. Have them bend and extend their legs leg 5-10 times at the knees.
- Plantar/dorsi flexion – have your client/patient lie on their back with both legs extended up toward the ceiling. Have them point and flex their feet at the ankle joint 5-10 times.
- Foot circles – have your client/patient lie on their back with both legs extended up toward the ceiling. Have them perform clockwise and counter-clockwise circumduction with both feet 5-10 times